Glaucoma
DMEK Outcomes after Glaucoma Surgery
What accounts for problems in these cases? Howard Larkin reports from the 2022 ASCRS Annual Meeting.

Howard Larkin
Published: Friday, August 5, 2022
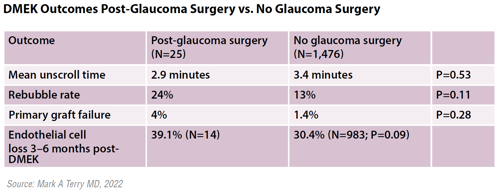
Rebubbling, primary graft failure, and endothelial cell loss rates all appeared to trend higher in a recent review of Descemet membrane endothelial keratoplasty (DMEK) performed after tube or trabeculectomy surgery, reported Mark A Terry MD at the 2022 ASCRS Annual Meeting.
In a study of 1,501 consecutive DMEK cases, the 25 performed after trabeculectomy or filtration tube surgery for glaucoma experienced more complications than those without previous glaucoma filtration surgery. But while the differences were notable, they did not rise to statistical significance, possibly due to the small post-glaucoma sample size.
One thing previous glaucoma surgery did not affect was unscrolling time during DMEK, Dr Terry said. Mean unscroll time in the post-glaucoma surgery group was 2.9±3.0 minutes compared with 3.4±5.2 minutes for the control group (p=0.53), indicating the DMEK surgery in post-glaucoma eyes was generally not any more difficult than in Fuchs’ dystrophy eyes.
Rebubbling rates were higher for the post-glaucoma group at 24% compared with 13% for the control group (p=0.11). Primary graft failure rates were 4% for the post-glaucoma surgery group compared with 1.4% for the control group (p=0.28). Endothelial cell loss three to six months after surgery came closest to statistical significance at 39.1% for the post-glaucoma surgery group and 30.4% for the control group (p=0.09).
Dr Terry’s rebubble rates are consistent with studies of postglaucoma surgery DMEK in the literature, while his endothelial cell loss and graft failure rates were about half that of other studies. They include a 2019 study finding a 22% rebubble rate, 71% endothelial cell loss, and 9% primary graft failure rate one year after DMEK in 23 patients with glaucoma drainage devices.i
“These cell loss and failure rates are high,” he said.
Another study reviewed 51 post-glaucoma surgery DMEK cases and found lower graft survival rates and higher endothelial cell loss rates at 12, 24, 36, and 48 months after DMEK compared with controls without previous glaucoma surgery.ii In a third study, 27 eyes with DMEK after a glaucoma drainage device also had lower graft survival rates and higher endothelial cell loss than 39 eyes with DMEK after trabeculectomy.iii
INFLAMMATION AND REDUCED AQUEOUS MAY PLAY A ROLE
Dr Terry discussed several possible reasons for the higher rates of rebubbling, primary graft failure, and endothelial cell loss for DMEK after glaucoma surgery. Rebubbling rates may be higher due to more frequent hypotony and loss of bubble support due to gas moving up the tube or bleb. Chronic inflammation and reduced aqueous nutritional support may also be factors affecting graft failure and endothelial cell loss.
i American Journal of Ophthalmology. 2019; 199: 150–158.
ii American Journal of Ophthalmology. 2020; 218: 7–16.
iii Graefe’s Archive for Clinical and Experimental Ophthalmology. 2022 May; 260(5): 1573–1582.
Mark A Terry MD is Director of Corneal Services at Devers Eye Institute and Professor of Clinical Ophthalmology at Oregon Health & Science University in Portland, Oregon, USA. mterry@deverseye.org
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.